Blog
The Benefits of Seeing a Podiatrist
- posted: Nov. 07, 2023
A podiatrist is a specialized medical professional devoted to the diagnosis, treatment, and care of conditions related to the feet, ankles, and lower extremities. Their expertise encompasses many issues, from Read More
The Benefits Of Orthotics
- posted: Nov. 01, 2023
Orthotics are custom-made shoe inserts or insoles designed to support and correct irregularities in foot function. They aim to alleviate various foot and ankle conditions, providing relief and improved mobility. Read More
When To See a Podiatrist
- posted: Oct. 06, 2023
A podiatrist is an expert at diagnosis and treatment of foot, ankle, and toe conditions. A podiatrist can help you enjoy healthy feet, so you can stay active. Visiting your Read More
The Importance of Diabetic Care
- posted: Oct. 01, 2023
When you’re dealing with diabetes, it’s important that you’re getting all the care that you need to ensure every part of your body. One big issue is making sure that Read More
Treating Your Bunion Symptoms
- posted: Sep. 14, 2023
Bunions are a common problem. In fact, over half of the women in the United States have developed a bunion at some point, according to the American Academy of Orthopedic Read More
Bunion Treatment Options
- posted: Sep. 01, 2023
If you have a bunion, you are not alone. A bunion is one of the most common, and painful foot problems your podiatrist can treat. What You Need To Know About Read More
When You Should See a Podiatrist for Ankle Pain
- posted: Aug. 09, 2023
Ankle pain can cause problems in your life. When you have ankle pain it can affect your ability to stand, put weight on your ankle, and walk around. Fortunately, your Read More
Foot Health for Children
- posted: Aug. 01, 2023
When you think about taking care of your child, you may not be thinking about taking care of your child’s feet. The truth is, foot health for children is important, Read More
Heel Pain: Causes and Treatments
- posted: Jul. 17, 2023
When you’re dealing with an issue like heel pain, this could be caused by a variety of issues. Each issue has different specific causes and symptoms and it’s important that Read More
Diabetes and Foot Care: Tips for Maintaining Healthy Feet
- posted: Jul. 01, 2023
Diabetes is a serious disease, affecting many of the major systems of your body, including your immune, circulatory, and nervous systems. The effects of diabetes are especially evident in your Read More
What To Do for Ankle Pain
- posted: Oct. 01, 2022
Your ankles are an important part of your body. Together with your legs and feet, your ankles help carry your body weight. They help you walk, run, and enjoy daily Read More
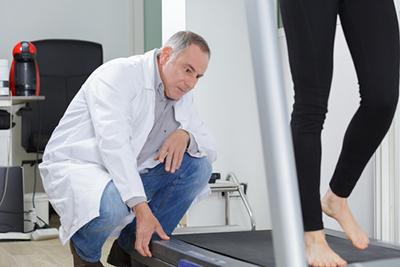
When To See a Podiatrist for a Sports Injury
- posted: Sep. 22, 2022
Sports injuries happen, and your feet and ankles are especially vulnerable. Your feet and ankles are overworked to begin with, and if you play a sport with a lot of Read More
Is My Toe Broken?
- posted: Sep. 01, 2022
Do you suspect that you might have broken your toe? You could very well be dealing with a broken toe if you notice pain, stiffness or swelling, or if you Read More
Hammertoes and Their Causes
- posted: Aug. 18, 2022
Discover more about this foot deformity and why it happens. Bunions always seem to get the spotlight when talking about foot deformities; however, it’s also essential to shed light on hammertoes. Read More
Common Causes Of Heel Pain
- posted: Aug. 09, 2022
Are you wondering what’s causing your heel pain? Heel pain is a real nuisance. When people turn to our Wilmette, IL, podiatrist Dr. Gary Rogers and the Wilmette Foot and Ankle Read More
Our Location
1919 Lake Ave Ste A
Wilmette, IL 60091-1480